Ozempic Lawsuit Information & Injury Lawyers
The Ozempic lawsuits claim Ozempic injections can cause acute gallbladder disease
Our law firm is not accepting cases but this page is to make you aware of the potential issues
What Do We Know About the Ozempic Acute Gallbladder Disease Lawsuits?

Semaglutide—the generic name for Ozempic—is a prescription drug used to control high blood sugar in individuals with type 2 diabetes mellitus. It is classified as a GLP-1 Receptor Agonist Analog-Type drug.
Adverse Event Reports to FDA
More than 10,000 semaglutide-related adverse events were reported to the FDA Adverse Reporting System (FAERS) through the fourth quarter of 2021, of which numerous of these adverse events were specificized as gallbladder-related disorders.
According to FAERS, all the reported cases of cholelithiasis (gallstones) were coded as serious adverse events. The Benefit-Risk Assessment in the Center for Drug Evaluation and Research’s (CDER) clinical review of Ozempic (September 6, 2017) speaks to the efficacy of the drug, while also acknowledging the drug’s safety profile being consistent with the “known safety profile” for GLP-1 RAs, “with gastrointestinal adverse events being the most common adverse events.”
What Clinical Trial Data Tells Us About Ozempic
According to the Ozempic product label, cholelithiasis (gallstones) was reported in 1.5% and 0.4% of 0.5 mg and 1 mg semaglutide-treated patients, respectively, compared to 0% of patients assigned a placebo. Four acute gallbladder events led to treatment discontinuation. These included 3 events of jaundice, cholelithiasis, and hydrocholecystitis with semaglutide 0.5 mg and 1 report of bile duct stone with placebo.
The Ozempic clinical trials resulted in 90% of patients reporting cholelithiasis coded as a serious event requiring cholecystectomy (gallbladder removal).
Ozempic Injuries and Side Effects
Studies have linked Ozempic to various gallbladder diseases, most notably cholelithiasis (gallstones) and cholecystitis (inflammation of the gallbladder).
Cholelithiasis
Cholelithiasis is another name for gallstones, deposits of hardened digestive fluid that manifest in the gallbladder. These deposits vary in size, sometimes growing to the size of a golf ball. A person who develops cholelithiasis can experience symptoms from one or multiple gallstones.
Signs and symptoms of gallstones generally arise when they settle in a duct, creating a blockage. These signs and symptoms can include:
Intensifying pain (rapid and sudden) in the abdomen (upper right or center)
Pain between the shoulder blades
Pain in the right shoulder
Nausea
Vomiting
Cholecystitis
Inflammation of the gallbladder is called cholecystitis. The gallbladder serves as a container for digestive fluid (bile) that releases into the small intestine, according to the Mayo Clinic. When gallstones form, they can block the tube that leads out from the bladder. The bile accumulates, inflaming the gallbladder.
This inflammation, if left untreated, can prompt life-threatening complications, including a gallbladder rupture. A common treatment for cholecystitis calls for removal of the organ.
Signs and symptoms of cholecystitis include:
Severe pain in the abdomen (upper right or center)
Pain between the shoulder blades
Abdomen is tender to the touch
Nausea
Vomiting
Fever
The Timeline Important to the Ozempic and Acute Gallbladder Disease Lawsuits

-
2012: Novo Nordisk develops Ozempic as a diabetes therapy offering a longer-acting alternative to liraglutide.
-
2016: Clinical trials of Ozempic begin.
-
2016: The FDA New Drug Application is filed.
-
2017: Clinical trials of Ozempic are completed in May.
-
2017: Ozempic is approved by the United States Food and Drug Administration (FDA) in December as an injectable form of semaglutide to improve glycemic control in adults with type 2 diabetes mellitus.
-
2017: University of Leeds researchers and Novo Nordisk report that semaglutide can be used to treat obesity.
-
2018: Ozempic is approved in the European Union, Japan, and Canada.
-
2019: Novo Nordisk’s Rybelsus (a form of semaglutide taken by mouth) is approved for medical use in the U.S.
-
2020: Rybelsus is approved for medical use in the European Union
-
2021: More than 10,000 semaglutide-related adverse events are reported to the FDA Adverse Reporting System (FAERS).
What Is the Purpose of Ozempic?

Ozempic is marketed as a non-insulin medication that controls blood sugar levels in patients with type 2 diabetes. The manufacturer promotes the drug as an avenue that can be taken by patients who struggle to meet their blood sugar goals. Also known as semaglutide, the drug works like a human glucagon-like peptide (GLP-1). It boosts insulin secretion, which increases sugar metabolism.
Novo Nordisk’s website cites the American Diabetes Association’s recommendation that for most adults with type 2 diabetes, an A1C of less than 7% is a “reasonable goal” and that Ozempic is proven to lower blood sugar and A1C.
According to the Ozempic website, the drug helps a patient’s pancreas release more insulin upon detecting high blood sugar levels. Reportedly, the drug also stops the patient’s liver from producing and releasing excessive amounts of sugar, and it slows down food leaving the patient’s stomach.
The Ozempic website also promotes that the drug “may help you lose some weight.” On average, adults who take the drug lose up to 12 pounds, according to the medicine’s website.
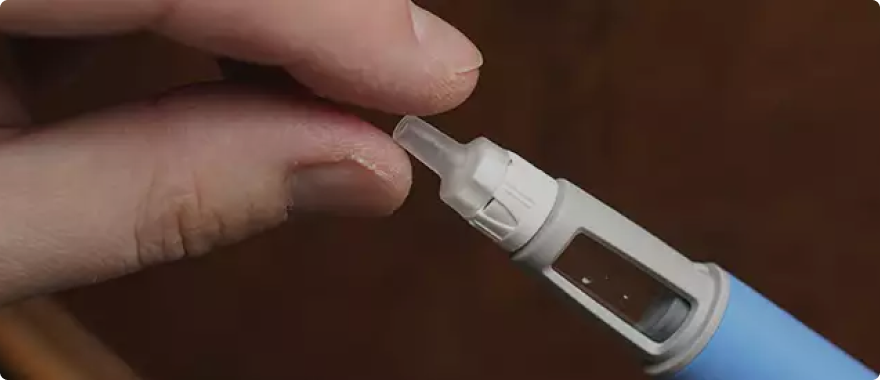
The medication is administered as a liquid through a prefilled pen, with patients taking one dose, once a week. Patients inject the drug once a week in their abdomen, thigh, or upper arm.
FDA & Scientific Studies Regarding Ozempic and Acute Gallbladder Disease

Association of Glucagon-Like Peptide-1 Receptor Agonist Use With Risk of Gallbladder and Biliary Diseases
This meta-analysis studied the link between GLP-1-1 RA treatment with gallbladder and biliary diseases and to explore risk factors for such associations. Researchers used randomized clinical trials to compare the use of GLP-1 RA drugs with placebo or with non-GLP-1 RA drugs in adults. The primary outcome was the composite of gallbladder or biliary diseases. Secondary outcomes were biliary diseases, biliary cancer, cholecystectomy, cholecystitis, and cholelithiasis.
The meta-analysis observed an increased risk of cholelithiasis (RR 1.27; 95% CI 1.10-1.47) and cholecystitis (RR 1.36; 95% CI 1.14-1.62) with GLP-1 RAs compared to placebo or active comparator. Researchers concluded that use of GLP-1 RAs was associated with increased risk of gallbladder or biliary diseases, especially when used at higher doses, for longer durations, and for weight loss. Read more at JAMA Internal Medicine.
Cholelithiasis in patients treated with Glucagon-Like Peptide-1 Receptor: An updated meta-analysis of randomized controlled trials
In this meta-analysis, researchers updated existing associations between GLP1-RA and cholelithiasis after the publication of new trials. As a result of the new analysis, researchers identified a significant increased risk of cholelithiasis with GLP-1 RAs (MH-OR 1.28; 95% CI 1.11-1.48) including in sensitivity analysis with continuity correction (MH-OR 1.26; 95% CI 1.10-1.45) compared to placebo or active comparator. Read more at Diabetes Res Clin Pract.
Safety issues with glucagon-like peptide-1 receptor agonists (pancreatitis, pancreatic cancer and cholelithiasis): Data from randomized controlled trials
This meta-analysis aimed to evaluate the effect of GLP1-RA on pancreatitis, pancreatic cancers, and cholelithiasis, taking into account the data from recently published cardiovascular outcome trials (CVOT) with GLP1-RA. Although prior meta-analyses did not show significant increase of risk of pancreatitis and pancreatic cancer with GLP1-RA, these efforts did not have the benefit of these newer bodies of data. The researchers in this meta-analysis concluded GLP1-RA was safe for pancreatitis, therapy using such drugs indicated an increased risk of cholelithiasis. Read more at Diabetes Obes Metab.
Association of Bile Duct and Gallbladder Diseases With the Use of Incretin-Based Drugs in Patients With Type 2 Diabetes Mellitus
This comparative study aimed to identify any associations with the use of DPP-4 inhibitors and GLP-1 analogues with an increased risk of gallbladder and incident bile duct disease in patients suffering from type 2 diabetes. The study revealed that 853 of 71,369 patients were hospitalized for bile duct and gallbladder disease, and researchers reported that the use of GLP-1 analogues was linked to an increased risk of these illnesses. GLP-1 analogues were also associated with an increased risk of cholecystectomy. Having concluded an increased risk of bile duct and gallbladder disease from the use of GLP-1 analogues, researchers cautioned physicians to be aware of such risks when prescribing these drugs. Read more at JAMA Intern Med.

AWARDS
Best Law Firms: U.S. News & World Report
Best Lawyers in America
National Trial Lawyers Hall of Fame
Public Justice Trial Team of the Year
Martindale-Hubbell Preeminent Woman Attorney
National Law Journal Elite Trial Lawyers
SuperLawyers

CLIENT STATEMENTS

You saved my life.

I want to express my deepest appreciation.

You mean so much to our family.

I am so appreciative.

To read our client reviews, visit our Testimonial page.
 (800) 277-1193
(800) 277-1193